|
I’m proud to announce my achievement as a sports certified specialist (SCS). This is a board-certified clinical specialist designation by the American Board of Physical Therapy Specialties (ABPTS) of the American Physical Therapy Association (APTA) in the area of Sports Rehabilitation. Specialist certification formally recognizes physical therapists who have demonstrated advanced clinical knowledge and skills in a specific area of physical therapist practice. As a sports specialized therapist, I have demonstrated both advanced clinical rehabilitation knowledge pertaining to sports injuries and sideline management of acute sports injuries. As a part of the certification process, I took training out of state to become an Emergency Medical Responder (EMR) through the American Red Cross where I learned and demonstrated proficiency in advanced first-aid techniques and acute injury management. The whole process, a little over a year in duration also included intense studying in current research and rehabilitation techniques for all areas of the body to return an individual back to a high level of activity. (This explains my lack of blog posts for the last year!)
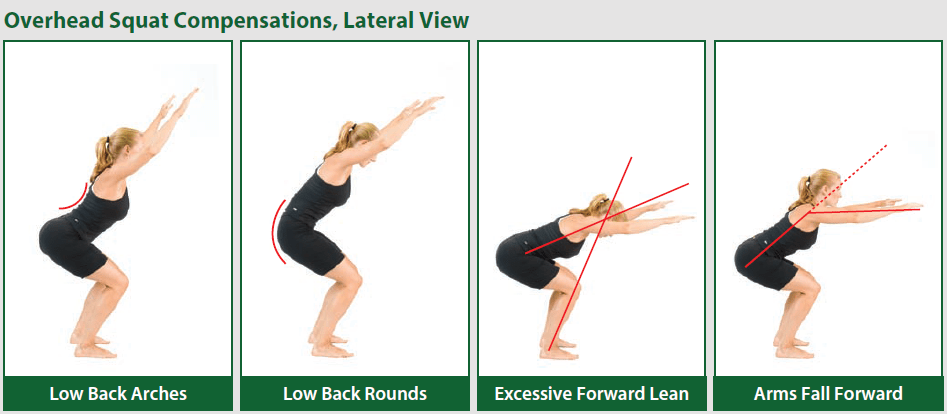
While I do get to add additional letters behind my name, it was never about this. This process was a great way to analyze strengths/weaknesses in my clinical practice and improve upon them. It also improved my use of evidence-based practice, which uses research to try to provide the best, most efficient treatments to help a condition. I believe in total, this process has allowed me to even further strengthen my skill set to provide the best treatments to help my patients the most. At the end of the day, that’s what it’s all about… helping those in need and forming trusting relationships. Whether you are an athlete, enjoy working out, or a desk jockey, the likeliness is you’ve experienced pain or discomfort at one point or another in your life. In many cases, these injuries will come and go in a relatively short time period and you don’t require treatment. But what about the injuries/pain that come and never fully recover or that keep coming back? This is where the skill of a physical therapist can come into play. Unfortunately, I think some people have misconceptions about what physical therapy is. Either they have had a negative experience in the past or feel “I don’t have time for therapy” as they think you need to devote multiple appointments a week for several weeks to treatment. I compare a physical therapist to a good lawyer. There are times where you might be in major trouble/conflict and need multiple visits to work something out, but other times you just need consultation and direction from time to time (or a tune-up). Also, just as all cars aren’t the same, all physical therapists aren’t the same. Unfortunately, there are still therapists out there using the “throw the kitchen sink at the patient and hope something works” technique. So where am I going here and how does this relate to functional movement assessment? A functional movement assessment has a patient perform multiple movements to systemically find the source of their dysfunction. This increases efficiency and effectiveness of treatment and there is a direct cause and effect relationship seen with activities/exercises! You see, I’m an impatient person, early in my career I never was really comfortable with the throw and wait technique. Just as you as a patient want to feel better, I as a therapist want more of an immediate result that I’m helping you. That’s why I get so excited about functional movement, dry needling, and cupping because when used together it can produce some of the quickest results I’ve seen as a therapist. Most of my patients need to see me 1-3 times to see major changes in their symptoms. The “homework” that you perform between visits work on exercises that are helping to build better movement patterns. As you get better with the movements, the stress on the injured area improves and your body has the ability to recover. Take the squat for example. Picture from www.thefitnesstraineracademy.org If you perform a squat and there is a flaw, this occurs for a reason and is likely putting extra stress on parts of your body. This can lead to INJURY and PAIN! These flaws may be the result of an injury or the cause of an injury. Just because you feel better after an injury doesn't mean all the effects of the injury are gone, hence why some people never feel "back to normal" after an injury. A functional movement assessment will break down the squat to determine why you are moving incorrectly and give you exercises that are components leading towards correcting these flaw(s). As your exercises progresses, your ability to perform a proper squat should also progress. Moving better means less stress on your body and your body is better at working as a machine. You should see a noticeable change not only in your ability to squat, but if addressing the appropriate mechanisms, YOUR SYMPTOMS! The original source of dysfunction, when optimized, becomes the exercise you need to build on to continue improving/maintaining the change. It’s the ultimate cause and effect relationship.
Contact me to discuss your personal functional movement assessment! Cupping therapy, although part of ancient Chinese medicine, was thrust into the limelight during the Rio Olympics. Although many of the athletes were being treated with cups, the American swimmers came out with circular red and purple marks which were visible on their skin. The announcers were obsessed with pointing out what the marks were and trying to explain the benefits of such treatment. New stories popped up on the internet claiming cupping was “pseudoscience”, “superstition”, and just the “latest fad” with pictures showing horrific burns. So what gives?
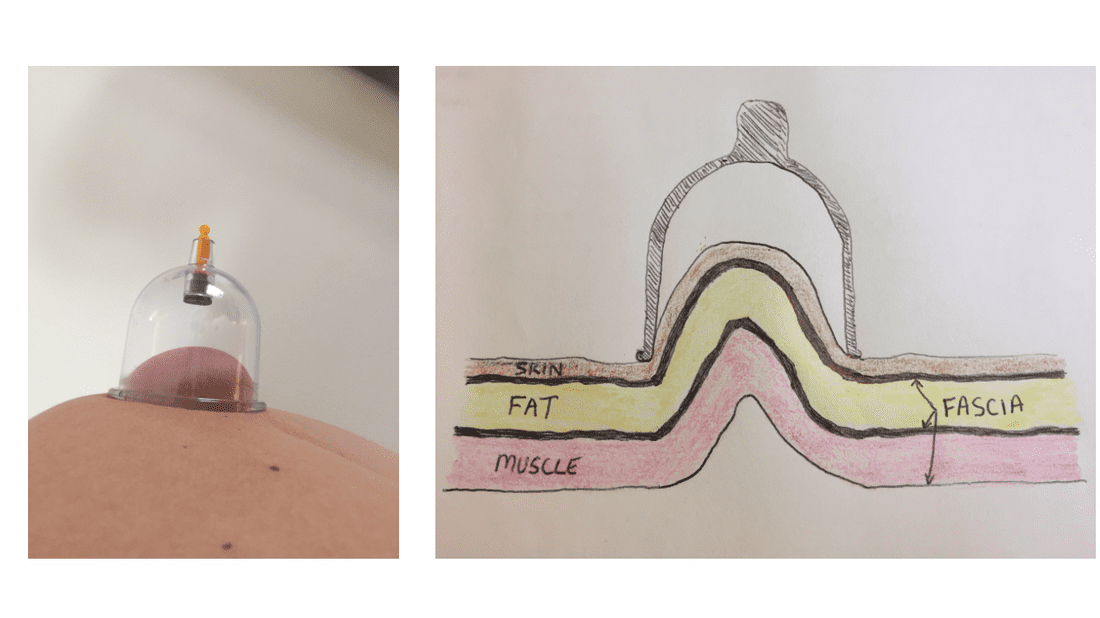
Let’s start by talking about what cupping therapy is. Cupping therapy involves placing a cup, which can be made out of different material ranging from plastic to glass. The general premise involves placing negative pressure under the cup forming suction. This can be achieved again through various means, but the most common is by a pump or by heating up the cup with fire just before placing on the skin. Although lighting something on fire is definitely more dramatic than adding a couple pulls to a plastic pump, I just don’t see the additional benefit of risking catching the clinic on fire, so I choose the plastic pump. Next, just as needling can be termed wet (with medication) or dry (without medication), cupping can be termed wet or dry. Wet cupping involves a form of bloodletting (cutting the skin and applying suction over the wound to suck out the bad, stagnant blood)-WHAT!?!? Umm no, no, no. Don’t get me wrong, if it works for you, great, but for some reason the “do no harm” vow that we take as medical professionals somehow feels broken when you slice open your patient just to watch them bleed. So let’s move on the the type of cupping that I perform, the dry version. Dry cupping again does NOT involve bleeding as a primary goal. The suction under the cup is thought to have many benefits, including: stretching tissue and fascia, increasing circulation and healing, and reducing pain just to name a few. The main reason I use cupping is for the stretching tissue effect, think of it like a deep tissue massage with much less time and effort. Where massage attempts to push through the layers to stretch the body, lengthening the tissue similar to rolling out dough with a roller, cupping pulls the tissue upward into the cup taking out the slack and providing a stretch (see pic above). The range of motion and flexibility gains after a simple treatment of cupping can be immediate and quite noticeable. Cupping techniques can vary according to the goal of treatment, but can involve simply placing the cups on the body and removing, moving the cups around once they are in place, or performing movements with your body while the cups are in place. So about the marks that the cups leave. They look like absolute torture right? So what does cupping feel like and how about those marks after treatment? When the cups are in place, think of an intense/effective stretch in the area targeted and then once the cups are removed, you tend to feel an immediate improvement in ease of movement and range of motion. The marks produced following may be a little sore to push on, but generally are not painful. They actually look much worse than they feel, with the patient not realizing they are even there after the treatment unless viewed. So prior to cupping, make sure you aren’t attending a wedding in a strapless dress and getting your neck/shoulders cupped! So why should I come to have cupping treatments performed with you instead of purchasing the $30 kits off Amazon and performing myself? First, when cupping is performed without training, serious bodily harm can occur if performed incorrectly! Also, just as with many other treatments, cupping is part of an overall treatment plan. Are the results permanent alone, probably not. After starting with a proper assessment, cupping can be combined with dry needling, stretching, or strengthening activities to target not only the symptom but the source. This is how you see results come your way. Do I have you interested……
Often I’m asked, why did you become a physical
therapist? I did not grow up thinking I always wanted to be a physical therapist, in fact like most kids, I was fascinated with planes and a pilot was probably what I said the most. As a son of a father who is an engineer, I did know what I didn’t want to be. You see, I was a hyper kid growing up, one that could never sit still, and the thought of sitting behind a desk at a computer in an office for 40 hours per week seemed dreadful. My father has dealt with low back pain and leg pain as far as I can remember. Frequently as a child, he asked me to walk on his back to try to help with his pain or he had mom massage his legs because of muscle spasms. He began having significant difficulty walking across the room, which led to his back surgery. It was hard for me growing up seeing him wanting to be involved in the games of baseball or basketball in the backyard, but either hurting too bad to attempt it or if he did, being laid up for a week recovering. I began going to his physical therapy appointments with him and quickly learned this is what I wanted to “do when I grow up.” The post I linked above is of major importance to me. Reading it alone is powerful, but looking deeper into the meaning is where I think it truly hits home. Often people thank me for “fixing” them, but I don’t view myself as a fixer or that I have this remarkable “gift”, I see myself as very passionate about what I do and like every physical therapist I like to help help people reach their goals. Sure there are treatments that require me doing something to you, but all in all, it’s just a step in the process of teaching you how to return to the things you want to do. A step to get me out of the picture and allow you to manage your symptoms or get rid of them all together. I want to get you back to spending more time and energy toward the ones you love or the things you love. It all comes back to why I got into therapy, helping dads get back to playing with kids in the backyard or kids returning to the sport they love. If you think I can help you reach your goals... |
AuthorRyan Goodman is owner of Goodman Performance Therapy LLC and the Team Physical Therapist for the Columbus Blue Jackets with experience in Orthopedic and Sports Medicine Injuries. Archives
November 2018
Categories
All
|


 RSS Feed
RSS Feed